"Jana basically walked me through how to get off the medication, and her method worked," maintains Tyrrell, who lives in suburban Chicago. "And thank goodness, because doctors don't understand this."
That's true all too often, Hill agrees. "These are controlled substances, and prescriptions are supposed to last for no more than a month — but some people are left on them for decades. So you can't blame the patient. You have to blame mis-prescribing."
This observation is seconded by Dr. Scott Shannon, a board-certified psychiatrist with The Wholeness Center, a Fort Collins clinic that specializes in assisting individuals dealing with the worst benzos symptoms; it's the only medical facility in Colorado recommended by the Benzodiazepine Information Coalition, widely acknowledged as the Internet's top resource for facts about this growing problem. (Tyrrell is on the coalition's board.) "I've been working in the area of integrated psychiatry for thirty years, training physicians to avoid these medications at all costs," Shannon points out. "But they're still given out like candy."
Benzos aren't addictive in the traditional sense; patients who discontinue use don't crave them. Rather, Shannon says, "it's a physical dependence. What happens is, the body accommodates to being on these things and then has difficulty coming off them. They have prolonged withdrawal issues, and some people, no matter how much support we give and other interventions we do, just aren't able to get off the medications."
Westword explored the potentially shocking repercussions of benzos related to the tragic case of John Patrick Walter, who died in Fremont County Jail in 2014. Walter had been taking Klonopin when he was arrested, but staffers at the facility abruptly cut off his access to the meds.

John Patrick Walter died in Fremont County Jail of acute benzodiazepine withdrawal in 2014.
Estate of John Patrick Walter
Tyrrell experienced similar symptoms. She'd been prescribed Klonopin for anxiety after the birth of her daughter and took it for several years before determining that it wasn't working anymore. So she went to her doctor, who had her taper off use over a four-week period — after which all hell broke loose.
"When I went off it that first week, the anxiety came back," Tyrrell says. "But it was such a severe form of anxiety. It was like I was put into extreme fight-or-flight mode, where I could not calm down for a second. My heart was racing, pounding out of my chest. My vision became very blurry. Lights from the windows hurt my eyes and sounds hurt my ears. The floor seemed to be moving beneath me, and I experienced a complete detachment from my environment. Everything seemed fake, plastic, and my arms and legs were jerking out from my body, beyond my control."
She notes, "I could only pace, because I felt this extreme inner agitation in me. I wasn't able to speak clearly. I struggled to find words, and I couldn't sleep. Sleep just stopped. I had been a mother, a teacher, just living a normal life, and all of a sudden, I wasn't even able to care for my kids or do any kind of household chores. It was completely disabling."
At that point, Tyrrell was put back on benzodiazepine with the idea of tapering off the pills more slowly — and, she says, "that's where Jana Hill came in."
Hill, a technical writer with a science background, had her own negative experience with benzos. She was prescribed the pills after an illness in her family, but suffered awful symptoms when attempting to stop. "I used every method I could find, and my doctor didn't know how to do it — and the person he referred me to made it even worse," she recalls. "He said, 'Reduce your dosage by 50 percent every week, but that's a recipe for what happened with John Patrick Walter. The consequences are the same as making an enormous cut in dosage, but that's the advice detox centers give. They might do a fine job on other drugs, but when they do it the same way with benzodiazepine, people get sicker than when they came in."
When more standard medical techniques failed her, Hill came up with her own approach — reducing the dosage at a much more deliberate rate. "It can take years," she allows.
In Tyrrell's case, it did — two and a half all together. And this journey required incredible patience. "The only way I was able to come off it and have it be bearable was to take a liquid form of benzodiazepine," she reveals. "I was taught to dilute it — and you'll see how I did it on the show. I used a scale. I used syringes. I would measure my dose and take out just .01 milligram every day. It's a very gradual reduction — so subtle your brain is allowed to kind of keep up with it as you're slowly coming off the medication. It's a much more gentle way, instead of cutting pills — a harsh cut of a quarter-milligram a day. Otherwise, your body is so dependent on the medication that it causes unbelievable symptoms that you wouldn't even think could happen."
Although Hill says she has patented what she calls her benzodiazepine micro-taper procedure, she doesn't currently have a website to promote her services. Instead, she prefers that people find her by way of online message boards and the like and then works in consultation with doctors, who are learning her tactics one patient at a time.
There are no shortage of them, the Wholeness Center's Shannon concedes. He cites an American Journal of Public Health report, "Increasing Benzodiazepine Prescriptions and Overdose Mortality in the United States, 1996–2013," which estimated that 13.5 million adults had been placed on benzos by the end of the study. "If they get ten prescriptions a year, that's over 100 million benzodiazepine prescriptions a year," he calculates. "And that was six years ago."
The Wholeness Center does prescribe psychiatric medication on occasion, he acknowledges, "but we've always been very careful about the risk-benefit ratio. And when we do prescribe them — and certainly ones like benzodiazepine — we're much more cautious. In my practice, we spend as much time getting people off psychiatric medication as putting them on."
The reason is simple: In Shannon's experience, "up to 50 percent of people who've been on benzodiazepines for more than a few months have great difficulty getting off. And those who've been on them for more than six months have notable cognitive declines: IQ tests, executive functions."
Today, Tyrrell, who finished her final taper seven months ago, is doing much better. But that doesn't mean she's symptom-free. "After that first four weeks, my ear started ringing, and it's never stopped since," she reveals. "It's just a reminder that you're not completely healed. There are people who've been off for quite a while that report they do get back to 100 percent, and that's what I'm clinging to. But there's no research, really, to let us know if this is permanent, and it's definitely an injury — although the real nightmare and damage begins after the medication has left your body. It has nothing to do with, 'Oh, I want to take it again.' It's a complete malfunction of your central nervous system."
She hopes the CNN special and other pieces about benzos will alert the medical profession to the issue, as well as to the right and wrong ways to deal with it. "We don't want doctors to panic when they see, 'Oh, there's a problem with benzos,' and rip people off their prescriptions or taper them too fast. If they think four weeks is safe, it's not. That's how I got injured."
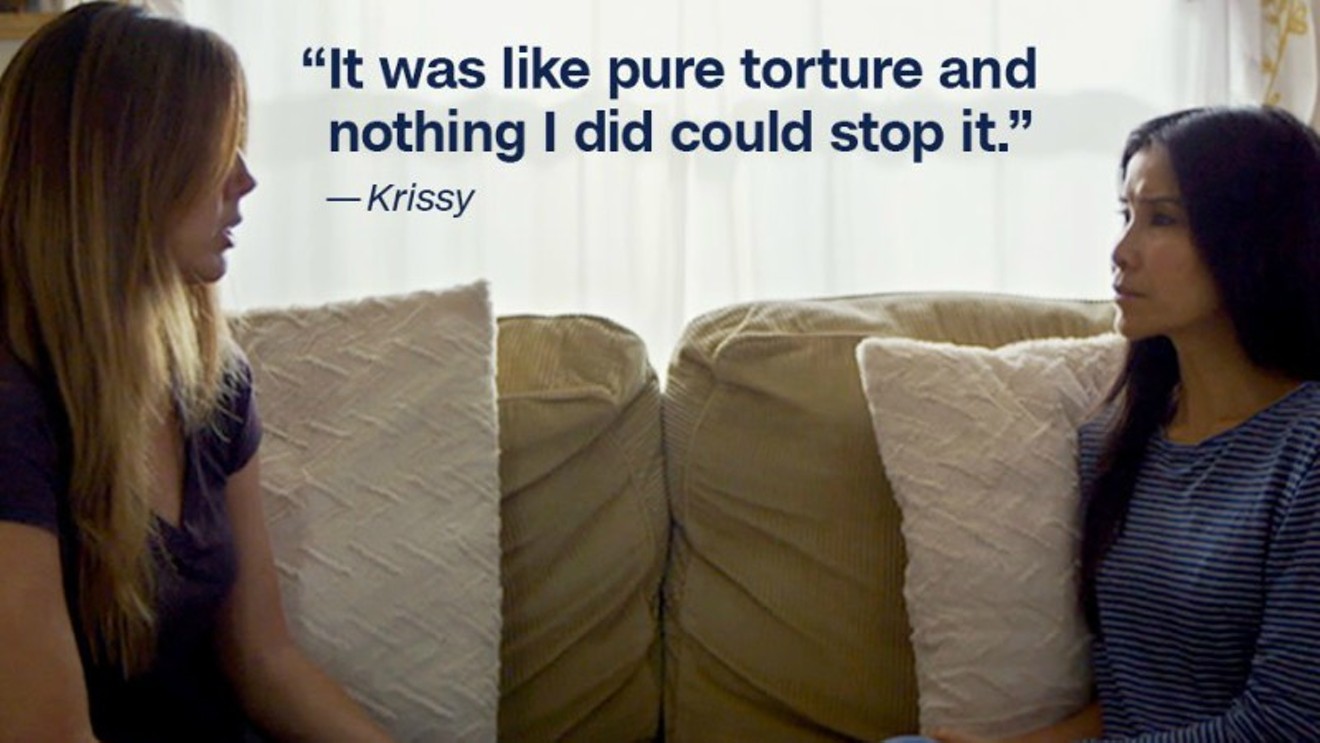
The benzodiazepine episode of This Is Life With Lisa Ling airs on CNN at 8 p.m. Mountain Time on Sunday, October 6.