Unfortunately, Crampton’s experience mirrors that of many emergency responders. A 2015 survey found that 86 percent of emergency medical services personnel reported critical stress (emotionally impactful stress, either built up over a career or the result of a single searing call); a job that entails frequent exposure to others’ once-in-a-lifetime tragedies takes a toll. But that truth can go unspoken, because the current workplace culture implicitly discourages discussing emotional trauma; unlike physical well-being and procedural familiarity, mental resiliency often isn't addressed in training. Instead, responders worry that if they reach out, co-workers will think they're too fragile for a tough job.
“In general, we are the helpers. We don’t ask for help. It’s seen as a sign of weakness,” explains Kelli Gilchrist, a Glendale-stationed firefighter who earned her master's in clinical counseling before joining the fire service and following in the footsteps of her father, a truck captain who served 37 years. But help, and openly prioritizing mental well-being as much as physical health, is definitely needed: From 2004 to 2014, Colorado lost 130 emergency responders (a term that includes law enforcement officers, dispatchers, EMS personnel and firefighters) to suicide. A Journal of Emergency Medical Services survey reported a suicide rate in EMS personnel ten times that of the general population, and high numbers are found among other emergency responders, too.
Even when emergency responders buck the stigma and decide to seek help in dealing with on-the-job exposure to trauma, their experiences often mirror Crampton’s. A therapist unfamiliar with the profession’s hierarchy might suggest speaking with a superior, unaware of the potential career-damaging ramifications. Other responders have had to spend a valuable chunk of therapy time simply explaining the fundamentals of their job or, worse yet, comforting a counselor shaken by the details of a particularly "bad call" (industry lingo for an emergency they helped resolve). And while peer-counseling programs, including the Denver Police Department's 35-year-old initiative, provide support (even preventing suicides) each year, sometimes emergency responders need to turn to a professional or someone unaffiliated with the workplace.

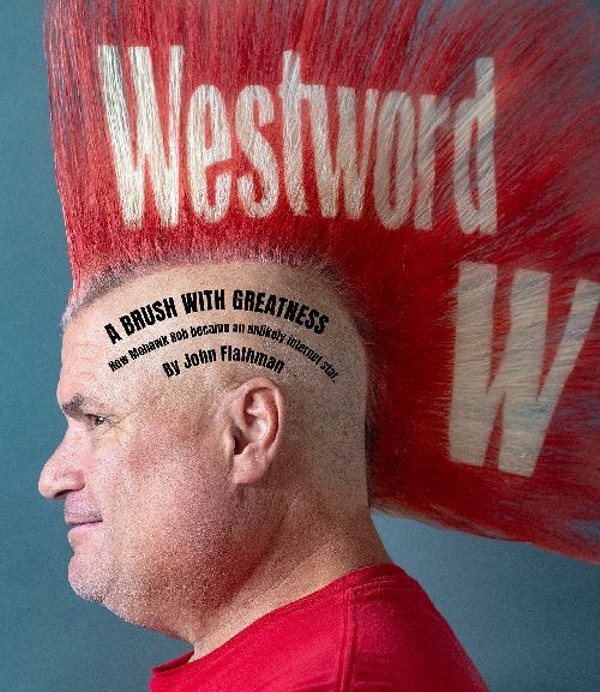
In this screenshot from the upcoming documentary Lifelines, paramedic Daniel Crampton (right) stands with a colleague.
Courtesy Status: Code 4, Inc.
Sheriffs-in-training run drills — “Go-go-go-go!” — down the hallway as the Counselor Academy gets started. The three emergency responders introduce themselves and the goal of the eight-hour, $150 training session: for the therapists in attendance to leave more culturally competent, with insight into the world of emergency responding and the mental-health challenges that exist within it, so they know how to better help their patients.
Cultural competence is a medical buzzword, commonly used when exhorting the importance of diversifying the field so that patients can get care from doctors who understand their background. For a realm as fraught with stigma and dependent upon patient-provider connection as mental health, this grasp on a patient’s culture is crucial. And take it from one of the Denver Fire Department’s own: “You have to be immersed in the culture to have buy-in,” says Gilchrist.
For the first half of the training, the emergency responders detail the ins and outs of their respective departments, from terminology to unique stressors to vibe. Crampton, who works for the Ute Pass Regional Ambulance District, explains with precision the neuroscience behind trauma-therapy technique, thanks to his doctorate in psychology. Coppedge has prototypical cop looks — bald pate and intimidating height — and tells lots of stories and jokes. Gilchrist, despite being sleep-deprived after a midnight call and then one at 5 a.m. that caught her in the shower so she had to rush to the engine still soapy, is energetic and sharply funny, poking fun at the other teachers as she does with her colleagues at the firehouse. “I’m going to be mean to you, and I’m going to mother you a little bit,” she says to the attendees, checking to make sure everyone's all right after Crampton shows graphic images of the kinds of injuries that emergency medical services personnel routinely encounter: skull fractures, car crashes, broken bones protruding from skin.
But the three don't rely solely on images and statistics: They share anecdotes from their own careers to explain the outlook of a population that looks at a map and sees a call they served at every street corner. They relate the calls that still haunt them, often those that fell closest to home. Coppedge broke down in 2005 when, for a training exercise, a friend asked him to comment on a ten-year-old recording that captured the events surrounding the line-of-duty death of a friend; both men’s wives had been pregnant at the time, and Coppedge had left the ICU as the soon-to-be widow headed in. Before that personal reckoning with the effects of trauma, “nobody had imparted it in a way I could understand,” he says. Now he plans to become a counselor once he retires from coordinating the department’s resiliency program and overseeing its training academy.
“In general, we are the helpers. We don’t ask for help. It’s seen as a sign of weakness.”
tweet this
For her part, Gilchrist still remembers how, on one of her first days back on duty after maternity leave, a frantic mother handed her a seizing baby. And those particularly horrible calls can linger in innocuous ways; the smell of cooking sausage, Crampton says, reminds him "as if it were yesterday" of a cardiac arrest call where the patient's skin was singed by a defibrillator during the paramedics' attempts to revive him.
The responders sketch out the challenges each subset of their population faces. For instance, dispatchers have to contend with a lack of closure; they have limited means to follow up and learn what happened to the many pleas for help that come in through their earpieces each day. Female emergency responders have to negotiate a male-dominated field, Gilchrist says, mentioning how unlike some of her colleagues, she has to work out consistently to maintain the upper-body strength her job requires. Cops, Coppedge shares, spend isolated, self-directed hours in a patrol car, and constantly addressing crime can leave veteran officers cynical about a world whose dark side they’re better acquainted with than most. Retired emergency responders are in a vulnerable mental state because they feel divorced from a fundamental part of their identity. And emergency medical services personnel who are employed by private ambulance services don't have the same retirement benefits that state-employed or unionized responders receive. For responders in the weightiest leadership roles, there's often nobody of similar rank to turn to.
But in spite of these differences, the teachers underline some commonalities among this group that's well-accustomed to the sound of sirens: a tough-it-out culture with a rigid chain of command, hyper-vigilance, the stress of how actions would play out to the public or media, and a type-A personality that makes a loss of control unsettling, whether in work situations or over their own emotions.
Gilchrist, who was in math class junior year at Columbine High School when two of her classmates opened fire, has seen her share of shoddy counseling, so she gives the therapists in attendance suggestions and cautions. “The window to help emergency responders is really small,” she warns, so it's critical to get it right, especially because if they've actually taken the scarily vulnerable step of talking to a therapist, the emotional strain is likely intense. Do, she advises, meet over coffee, rather than in a formal office setting, and foster friendships outside of the field. Don’t use fluffy-sounding therapy language — talk about the “brain” or “total wellness” instead — or act over-awed by an emergency responder’s job.
All three teachers discuss the coping mechanisms, including dark humor. “If you can’t cry,” reasons Coppedge, “you laugh.” They note the common problem of marital discord (Gilchrist says she's lucky: Her husband, also a firefighter, understands what she's seen on the days when she brings home takeout burritos for dinner), and how the adrenaline crash after a long (sometimes even 48-hour) shift means an emergency responder might slump in front of the television nursing a beer, physical and mental exhaustion mistaken by their loved ones for apathy. And they point out signs that warn that a responder’s resilience has worn thin, like taking unnecessary risks on the job or relying too much on booze to provide stress relief off-duty.
As the day slips into afternoon, the three therapists take notes and ask questions of the responders, who prompt them to offer feedback so they can scale and improve these trainings for the future. For one, Angie Christianson, noticing the mental-health challenges that confront emergency responders actually propelled her to pursue counseling. While serving up espresso drinks in Aurora, Christianson befriended and subsequently went on ride-alongs with emergency responders; on the morning of July 20, 2012, she saw them come in with blood-spattered uniforms after the theater shooting, making time for a coffee break with colleagues despite enduring obvious stress. Seeing that blend of trauma and resiliency inspired her to enroll in graduate counseling studies at the University of Colorado Denver, where she focuses on mental well-being in the emergency-responder community. In the process, she became a counseling intern at Building Warriors and joined ResponderStrong, an initiative of the National Mental Health Innovation Center to prioritize mental wellness among emergency responders that's headed by former firefighter/paramedic Rhonda Kelly. (Coppedge, Crampton and Gilchrist are also active ResponderStrong members.)“We don’t want people to go out bitter and broken, mentally or physically."
tweet this
The group in the classroom on this Saturday and the 500 people who make up ResponderStrong want to turn the silence around mental health into a robust discussion and "take care of the little stuff while it's still little," says Gilchrist. After all, as Coppedge tells the cops he mentors, it takes a stronger person to go against the culture and seek help than to go with it. Most of all, they want to prevent moments like those Crampton experienced, standing at the casket of an ambulance partner who died by suicide, oscillating between anger and sadness at his death.
As Kelly, the project manager for ResponderStrong, puts it: “We don’t want people to go out bitter and broken, mentally or physically."
For immediate help, call the Suicide Prevention Lifeline at 1-800-273-TALK (8255) or text Crisis Text Line at 741741. For Colorado-specific resources and support, visit coloradocrisisservices.org. And to find out more or get involved with Building Warriors (buildingwarriors.net; Facebook), ResponderStrong (responderstrong.org; Facebook) or Foundation 1023, which provides free-of-charge counseling to emergency responders in Colorado and Texas (foundation1023.org; Facebook), visit their websites or Facebook pages.